Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317:1517.
Google Scholar
American Psychiatric Association. Multiaxial assessment.DSM-IV-TR: diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association; 2002.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40.
Google Scholar
Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME, et al. Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N Engl J Med. 2006;354:1231–42.
Google Scholar
Fried EI, Nesse RM. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR*D study. J Affect Disord. 2015;172:96–102.
Google Scholar
Uher R, Perlis RH, Henigsberg N, Zobel A, Rietschel M, Mors O, et al. Depression symptom dimensions as predictors of antidepressant treatment outcome: replicable evidence for interest-activity symptoms. Psychol Med. 2012;42:967–80.
Google Scholar
Halahakoon DC, Kieslich K, O’Driscoll C, Nair A, Lewis G, Roiser JP. Reward-processing behavior in depressed participants relative to healthy volunteers: a systematic review and meta-analysis. JAMA Psychiatry. 2020;77:1286–95.
Google Scholar
Treadway MT, Bossaller NA, Shelton RC, Zald DH. Effort-based decision-making in major depressive disorder: a translational model of motivational anhedonia. J Abnorm Psychol. 2012;121:553–8.
Google Scholar
Yang X-H, Huang J, Zhu C-Y, Wang Y-F, Cheung EFC, Chan RCK, et al. Motivational deficits in effort-based decision making in individuals with subsyndromal depression, first-episode and remitted depression patients. Psychiatry Res. 2014;220:874–82.
Google Scholar
Cléry-Melin M-L, Schmidt L, Lafargue G, Baup N, Fossati P, Pessiglione M. Why don’t you try harder? An investigation of effort production in major depression. PLOS ONE. 2011;6:e23178.
Google Scholar
Costello H, Yamamori Y, Reeves S, Schrag A, Howard R, Roiser JP. Longitudinal decline in striatal dopamine transporter binding in Parkinson’s disease: associations with apathy and anhedonia. J Neurol Neurosurg Psychiatry. 2023;94:863–70.
Peciña M, Sikora M, Avery ET, Heffernan J, Peciña S, Mickey BJ, et al. Striatal dopamine D2/3 receptor-mediated neurotransmission in major depression: implications for anhedonia, anxiety and treatment response. Eur Neuropsychopharmacol. 2017;27:977–86.
Google Scholar
Salamone JD, Yohn SE, López-Cruz L, San Miguel N, Correa M. Activational and effort-related aspects of motivation: neural mechanisms and implications for psychopathology. Brain J Neurol. 2016;139:1325–47.
Google Scholar
Treadway MT, Buckholtz JW, Cowan RL, Woodward ND, Li R, Ansari MS, et al. Dopaminergic mechanisms of individual differences in human effort-based decision-making. J Neurosci. 2012;32:6170–6.
Google Scholar
Westbrook A, van den Bosch R, Määttä JI, Hofmans L, Papadopetraki D, Cools R, et al. Dopamine promotes cognitive effort by biasing the benefits versus costs of cognitive work. Science. 2020;367:1362–6.
Google Scholar
Maron E, Eller T, Vasar V, Nutt DJ. Effects of bupropion augmentation in escitalopram-resistant patients with major depressive disorder: an open-label, naturalistic study. J Clin Psychiatry. 2009;70:1054–6.
Google Scholar
Argyropoulos SV, Nutt DJ. Anhedonia revisited: is there a role for dopamine-targeting drugs for depression? J Psychopharmacol. 2013;27:869–77.
Google Scholar
Sacheli MA, Murray DK, Vafai N, Cherkasova MV, Dinelle K, Shahinfard E, et al. Habitual exercisers versus sedentary subjects with Parkinson’s disease: multimodal PET and fMRI study. Mov Disord Off J Mov Disord Soc. 2018;33:1945–50.
Google Scholar
Sacheli MA, Neva JL, Lakhani B, Murray DK, Vafai N, Shahinfard E, et al. Exercise increases caudate dopamine release and ventral striatal activation in Parkinson’s disease. Mov Disord Off J Mov Disord Soc. 2019;34:1891–1900.
Google Scholar
Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175:631–48.
Google Scholar
Morres ID, Hatzigeorgiadis A, Stathi A, Comoutos N, Arpin-Cribbie C, Krommidas C, et al. Aerobic exercise for adult patients with major depressive disorder in mental health services: a systematic review and meta-analysis. Depress Anxiety. 2019;36:39–53.
Google Scholar
Bailey AP, Hetrick SE, Rosenbaum S, Purcell R, Parker AG. Treating depression with physical activity in adolescents and young adults: a systematic review and meta-analysis of randomised controlled trials. Psychol Med. 2018;48:1068–83.
Google Scholar
Krogh J, Nordentoft M, Sterne JAC, Lawlor DA. The effect of exercise in clinically depressed adults: systematic review and meta-analysis of randomized controlled trials. J Clin Psychiatry. 2011;72:529–38.
Google Scholar
Shilyansky C, Williams LM, Gyurak A, Harris A, Usherwood T, Etkin A. Effect of antidepressant treatment on cognitive impairments associated with depression: a randomised longitudinal study. Lancet Psychiatry. 2016;3:425–35.
Google Scholar
Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci. 2003;14:125–30.
Google Scholar
Oertel-Knöchel V, Mehler P, Thiel C, Steinbrecher K, Malchow B, Tesky V, et al. Effects of aerobic exercise on cognitive performance and individual psychopathology in depressive and schizophrenia patients. Eur Arch Psychiatry Clin Neurosci. 2014;264:589–604.
Google Scholar
Rock P, Roiser J, Riedel W, Blackwell A, Rock PL, Roiser JP, et al. Cognitive impairment in depression: a systematic review and meta-analysis. Psychol Med. 2013;44:1–12.
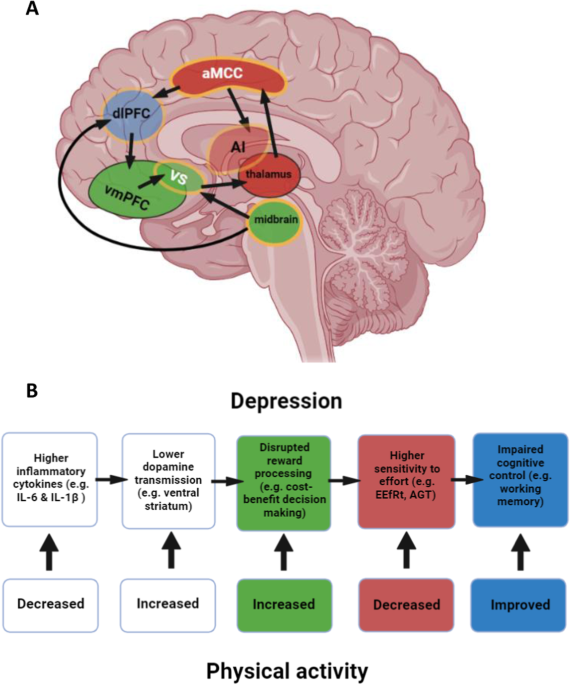
Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. 2019;107:525–39.
Google Scholar
Szuhany KL, Bugatti M, Otto MW. A meta-analytic review of the effects of exercise on brain-derived neurotrophic factor. J Psychiatr Res. 2015;60:56–64.
Google Scholar
Gujral S, Aizenstein H, Reynolds CF, Butters MA, Grove G, Karp JF, et al. Exercise for depression: a feasibility trial exploring neural mechanisms. Am J Geriatr Psychiatry. 2019;27:611–6.
Google Scholar
Schuch FB, Vasconcelos-Moreno MP, Borowsky C, Zimmermann AB, Wollenhaupt-Aguiar B, Ferrari P, et al. The effects of exercise on oxidative stress (TBARS) and BDNF in severely depressed inpatients. Eur Arch Psychiatry Clin Neurosci. 2014;264:605–13.
Google Scholar
Alghadir AH, Gabr SA. Hormonal function responses to moderate aerobic exercise in older adults with depression. Clin Interv Aging. 2020;15:1271–83.
Google Scholar
Beserra AHN, Kameda P, Deslandes AC, Schuch FB, Laks J, Moraes HSde. Can physical exercise modulate cortisol level in subjects with depression? A systematic review and meta-analysis. Trends Psychiatry Psychother. 2018;40:360–8.
Google Scholar
Schuch FB, Deslandes AC, Stubbs B, Gosmann NP, Silva CTBda, Fleck MPdeA. Neurobiological effects of exercise on major depressive disorder: a systematic review. Neurosci Biobehav Rev. 2016;61:1–11.
Google Scholar
Heinze K, Cumming J, Dosanjh A, Palin S, Poulton S, Bagshaw AP, et al. Neurobiological evidence of longer-term physical activity interventions on mental health outcomes and cognition in young people: a systematic review of randomised controlled trials. Neurosci Biobehav Rev. 2021;120:431–41.
Google Scholar
Robert P, Onyike CU, Leentjens AFG, Dujardin K, Aalten P, Starkstein S, et al. Proposed diagnostic criteria for apathy in Alzheimer’s disease and other neuropsychiatric disorders. Eur Psychiatry. 2009;24:98–104.
Google Scholar
Treadway MT, Zald DH. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci Biobehav Rev. 2011;35:537–55.
Google Scholar
Zald DH, Treadway MT. Reward processing, neuroeconomics, and psychopathology. Annu Rev Clin Psychol. 2017;13:471–95.
Google Scholar
Rømer Thomsen K, Whybrow PC, Kringelbach ML. Reconceptualizing anhedonia: novel perspectives on balancing the pleasure networks in the human brain. Front Behav Neurosci. 2015;9:49.
Google Scholar
Der-Avakian A, Markou A. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci. 2012;35:68–77.
Google Scholar
Pizzagalli DA. Depression, stress, and anhedonia: toward a synthesis and integrated model. Annu Rev Clin Psychol. 2014;10:393–423.
Google Scholar
Costello H, Husain M, Roiser J. Apathy and motivation: biological basis and drug treatment. 2023. https://doi.org/10.31234/osf.io/m3vjy.
Vrieze E, Pizzagalli DA, Demyttenaere K, Hompes T, Sienaert P, de Boer P, et al. Reduced reward learning predicts outcome in major depressive disorder. Biol Psychiatry. 2013;73:639–45.
Google Scholar
Pizzagalli DA, Iosifescu D, Hallett LA, Ratner KG, Fava M. Reduced hedonic capacity in major depressive disorder: evidence from a probabilistic reward task. J Psychiatr Res. 2008;43:76–87.
Google Scholar
Huys QJ, Pizzagalli DA, Bogdan R, Dayan P. Mapping anhedonia onto reinforcement learning: a behavioural meta-analysis. Biol Mood Anxiety Disord. 2013;3:12.
Google Scholar
Pechtel P, Dutra SJ, Goetz EL, Pizzagalli DA. Blunted reward responsiveness in remitted depression. J Psychiatr Res. 2013;47:1864–9.
Google Scholar
Kieslich K, Valton V, Roiser JP. Pleasure, reward value, prediction error and anhedonia. In: Pizzagalli DA, (ed). Anhedonia: preclinical, translational, and clinical integration. Cham: Springer International Publishing; 2022. p. 281–304.
Google Scholar
Husain M, Roiser JP. Neuroscience of apathy and anhedonia: a transdiagnostic approach. Nat Rev Neurosci. 2018;19:470–84.
Google Scholar
Pizzagalli DA, Holmes AJ, Dillon DG, Goetz EL, Birk JL, Bogdan R, et al. Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. Am J Psychiatry. 2009;166:702–10.
Google Scholar
Knutson B, Bhanji JP, Cooney RE, Atlas LY, Gotlib IH. Neural responses to monetary incentives in major depression. Biol Psychiatry. 2008;63:686–92.
Google Scholar
Gorka SM, Huggins AA, Fitzgerald DA, Nelson BD, Phan KL, Shankman SA. Neural response to reward anticipation in those with depression with and without panic disorder. J Affect Disord. 2014;164:50–56.
Google Scholar
Stringaris A, Vidal-Ribas Belil P, Artiges E, Lemaitre H, Gollier-Briant F, Wolke S, et al. The brain’s response to reward anticipation and depression in adolescence: dimensionality, specificity, and longitudinal predictions in a community-based sample. Am J Psychiatry. 2015;172:1215–23.
Google Scholar
Yadid G, Friedman A. Dynamics of the dopaminergic system as a key component to the understanding of depression. Prog Brain Res. 2008;172:265–86.
Dunlop BW, Nemeroff CB. The role of dopamine in the pathophysiology of depression. Arch Gen Psychiatry. 2007;64:327–37.
Google Scholar
Haber SN, Knutson B. The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacology. 2010;35:4–26.
Google Scholar
Salamone JD, Correa M. The mysterious motivational functions of mesolimbic dopamine. Neuron. 2012;76:470–85.
Google Scholar
Cooper JA, Arulpragasam AR, Treadway MT. Anhedonia in depression: biological mechanisms and computational models. Curr Opin Behav Sci. 2018;22:128–35.
Google Scholar
Rzepa E, Fisk J, McCabe C. Blunted neural response to anticipation, effort and consummation of reward and aversion in adolescents with depression symptomatology. J Psychopharmacol. 2017;31:303–11.
Google Scholar
Ubl B, Kuehner C, Kirsch P, Ruttorf M, Diener C, Flor H. Altered neural reward and loss processing and prediction error signalling in depression. Soc Cogn Affect Neurosci. 2015;10:1102–12.
Google Scholar
Liu W, Chan RCK, Wang L, Huang J, Cheung EFC, Gong Q, et al. Deficits in sustaining reward responses in subsyndromal and syndromal major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1045–52.
Google Scholar
Chase HW, Frank MJ, Michael A, Bullmore ET, Sahakian BJ, Robbins TW. Approach and avoidance learning in patients with major depression and healthy controls: relation to anhedonia. Psychol Med. 2010;40:433–40.
Google Scholar
Rothkirch M, Tonn J, Köhler S, Sterzer P. Neural mechanisms of reinforcement learning in unmedicated patients with major depressive disorder. Brain J Neurol. 2017;140:1147–57.
Google Scholar
Wardenaar KJ, Giltay EJ, van Veen T, Zitman FG, Penninx BWJH. Symptom dimensions as predictors of the two-year course of depressive and anxiety disorders. J Affect Disord. 2012;136:1198–203.
Google Scholar
Spijker J, Bijl RV, de Graaf R, Nolen WA. Determinants of poor 1-year outcome of DSM-III-R major depression in the general population: results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Acta Psychiatr Scand. 2001;103:122–30.
Google Scholar
McMakin DL, Olino TM, Porta G, Dietz LJ, Emslie G, Clarke G, et al. Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor treatment-resistant depression. J Am Acad Child Adolesc Psychiatry. 2012;51:404–11.
Google Scholar
Nutt D, Demyttenaere K, Janka Z, Aarre T, Bourin M, Canonico PL, et al. The other face of depression, reduced positive affect: the role of catecholamines in causation and cure. J Psychopharmacol. 2007;21:461–71.
Google Scholar
Padala PR, Padala KP, Monga V, Ramirez DA, Sullivan DH. Reversal of SSRI-associated apathy syndrome by discontinuation of therapy. Ann Pharmacother. 2012;46:e8.
Google Scholar
Fava M, Ball S, Nelson JC, Sparks J, Konechnik T, Classi P, et al. Clinical relevance of fatigue as a residual symptom in major depressive disorder. Depress Anxiety. 2014;31:250–7.
Google Scholar
Treadway MT, Buckholtz JW, Schwartzman AN, Lambert WE, Zald DH. Worth the ‘EEfRT’? The effort expenditure for rewards task as an objective measure of motivation and anhedonia. PloS One. 2009;4:e6598.
Google Scholar
Salamone JD, Correa M, Farrar A, Mingote SM. Effort-related functions of nucleus accumbens dopamine and associated forebrain circuits. Psychopharmacology. 2007;191:461–82.
Google Scholar
Bonnelle V, Veromann K-R, Burnett Heyes S, Lo Sterzo E, Manohar S, Husain M. Characterization of reward and effort mechanisms in apathy. J Physiol Paris. 2015;109:16–26.
Google Scholar
Chong T-T-J, Bonnelle V, Husain M. Quantifying motivation with effort- based decision-making paradigms in health and disease. Prog Brain Res. 2016;229:71–100.
Chong TT-J, Bonnelle V, Manohar S, Veromann K-R, Muhammed K, Tofaris GK, et al. Dopamine enhances willingness to exert effort for reward in Parkinson’s disease. Cortex J Devoted Study Nerv Syst Behav. 2015;69:40–46.
Google Scholar
Bonnelle V, Manohar S, Behrens T, Husain M. Individual differences in premotor brain systems underlie behavioral apathy. Cereb Cortex. 2015;26:bhv247.
Google Scholar
Shenhav A, Musslick S, Lieder F, Kool W, Griffiths TL, Cohen JD, et al. Toward a rational and mechanistic account of mental effort. Annu Rev Neurosci. 2017;40:99–124.
Google Scholar
Botvinick MM, Cohen JD. The computational and neural basis of cognitive control: charted territory and new frontiers. Cogn Sci. 2014;38:1249–85.
Google Scholar
Grahek I, Shenhav A, Musslick S, Krebs RM, Koster EHW. Motivation and cognitive control in depression. Neurosci Biobehav Rev. 2019;102:371–81.
Google Scholar
Marchetti I, Shumake J, Grahek I, Koster EHW. Temperamental factors in remitted depression: the role of effortful control and attentional mechanisms. J Affect Disord. 2018;235:499–505.
Google Scholar
Rock PL, Roiser JP, Riedel WJ, Blackwell AD. Cognitive impairment in depression: a systematic review and meta-analysis. Psychol Med. 2014;44:2029–40.
Google Scholar
Disner SG, Beevers CG, Haigh EAP, Beck AT. Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci. 2011;12:467–77.
Google Scholar
Gotlib IH, Joormann J. Cognition and depression: current status and future directions. Annu Rev Clin Psychol. 2010;6:285–312.
Google Scholar
Snyder HR. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychol Bull. 2013;139:81–132.
Google Scholar
Rayner G, Jackson G, Wilson S. Cognition-related brain networks underpin the symptoms of unipolar depression: Evidence from a systematic review. Neurosci Biobehav Rev. 2016;61:53–65.
Google Scholar
Laplane D, Levasseur M, Pillon B, Dubois B, Baulac M, Mazoyer B, et al. Obsessive-compulsive and other behavioural changes with bilateral basal ganglia lesions. A neuropsychological, magnetic resonance imaging and positron tomography study. Brain J Neurol. 1989;112:699–725.
Google Scholar
Adam R, Leff A, Sinha N, Turner C, Bays P, Draganski B, et al. Dopamine reverses reward insensitivity in apathy following globus pallidus lesions. Cortex J Devoted Study Nerv Syst Behav. 2013;49:1292–303.
Google Scholar
Manohar SG, Husain M. Human ventromedial prefrontal lesions alter incentivisation by reward. Cortex. 2016;76:104–20.
Google Scholar
Kang SY, Kim JS. Anterior cerebral artery infarction: stroke mechanism and clinical-imaging study in 100 patients. Neurology. 2008;70:2386–93.
Google Scholar
Le Heron C, Apps MaJ, Husain M. The anatomy of apathy: a neurocognitive framework for amotivated behaviour. Neuropsychologia. 2018;118:54–67.
Google Scholar
Pessiglione M, Vinckier F, Bouret S, Daunizeau J, Le Bouc R. Why not try harder? Computational approach to motivation deficits in neuro-psychiatric diseases. Brain J Neurol. 2018;141:629–50.
Google Scholar
Hauser TU, Eldar E, Dolan RJ. Separate mesocortical and mesolimbic pathways encode effort and reward learning signals. Proc Natl Acad Sci USA. 2017;114:E7395–E7404.
Google Scholar
Skvortsova V, Palminteri S, Pessiglione M. Learning to minimize efforts versus maximizing rewards: computational principles and neural correlates. J Neurosci. 2014;34:15621–30.
Google Scholar
Kroemer NB, Guevara A, Ciocanea Teodorescu I, Wuttig F, Kobiella A, Smolka MN. Balancing reward and work: anticipatory brain activation in NAcc and VTA predict effort differentially. NeuroImage. 2014;102:510–9.
Google Scholar
Suzuki S, Lawlor VM, Cooper JA, Arulpragasam AR, Treadway MT. Distinct regions of the striatum underlying effort, movement initiation and effort discounting. Nat Hum Behav. 2021;5:378–88.
Google Scholar
Parvizi J, Rangarajan V, Shirer WR, Desai N, Greicius MD. The will to persevere induced by electrical stimulation of the human cingulate gyrus. Neuron. 2013;80:1359–67.
Google Scholar
Croxson PL, Walton ME, O’Reilly JX, Behrens TEJ, Rushworth MFS. Effort-based cost–benefit valuation and the human brain. J Neurosci. 2009;29:4531–41.
Google Scholar
Kurniawan IT, Guitart-Masip M, Dayan P, Dolan RJ. Effort and valuation in the brain: the effects of anticipation and execution. J Neurosci. 2013;33:6160–9.
Google Scholar
Chong TT-J, Apps M, Giehl K, Sillence A, Grima LL, Husain M. Neurocomputational mechanisms underlying subjective valuation of effort costs. PLoS Biol. 2017;15:e1002598.
Google Scholar
Klein-Flügge MC, Kennerley SW, Friston K, Bestmann S. Neural signatures of value comparison in human cingulate cortex during decisions requiring an effort-reward trade-off. J Neurosci. 2016;36:10002–15.
Google Scholar
Shenhav A, Botvinick MM, Cohen JD. The expected value of control: an integrative theory of anterior cingulate cortex function. Neuron. 2013;79:217–40.
Google Scholar
Pizzagalli DA. Frontocingulate dysfunction in depression: toward biomarkers of treatment response. Neuropsychopharmacology. 2011;36:183–206.
Google Scholar
Davidson RJ, Pizzagalli D, Nitschke JB, Putnam K. Depression: perspectives from affective neuroscience. Annu Rev Psychol. 2002;53:545–74.
Google Scholar
Gotlib IH, Hamilton JP. Neuroimaging and depression: current status and unresolved issues. Curr Dir Psychol Sci. 2008;17:159–63.
Google Scholar
Eickhoff SB, Etkin A, Huemer J, Carreon DM, Jiang Y, McTeague LM. Identification of common neural circuit disruptions in cognitive control across psychiatric disorders. Am J Psychiatry. 2017;174:676–85.
Google Scholar
Nord CL, Halahakoon DC, Limbachya T, Charpentier C, Lally N, Walsh V, et al. Neural predictors of treatment response to brain stimulation and psychological therapy in depression: a double-blind randomized controlled trial. Neuropsychopharmacology. 2019;44:1613–22.
Google Scholar
Armbruster-Genç DJN, Valton V, Neil L, Vuong V, Freeman ZCL, Packer KC, et al. Altered reward and effort processing in children with maltreatment experience: a potential indicator of mental health vulnerability. Neuropsychopharmacology. 2022;47:1063–70.
Google Scholar
Sadaghiani S, D’Esposito M. Functional characterization of the cingulo-opercular network in the maintenance of tonic alertness. Cereb Cortex. 2015;25:2763–73.
Google Scholar
Han SW, Eaton HP, Marois R. Functional fractionation of the cingulo-opercular network: alerting insula and updating cingulate. Cereb Cortex. 2019;29:2624–38.
Google Scholar
Seeley WW. The salience network: a neural system for perceiving and responding to homeostatic demands. J Neurosci. 2019;39:9878–82.
Google Scholar
Hamid AA, Pettibone JR, Mabrouk OS, Hetrick VL, Schmidt R, Vander Weele CM, et al. Mesolimbic dopamine signals the value of work. Nat Neurosci. 2016;19:117–26.
Google Scholar
Sarchiapone M, Carli V, Camardese G, Cuomo C, Di Giuda D, Calcagni M-L, et al. Dopamine transporter binding in depressed patients with anhedonia. Psychiatry Res. 2006;147:243–8.
Google Scholar
Wardle MC, Treadway MT, Mayo LM, Zald DH, de Wit H. Amping up effort: effects of d-amphetamine on human effort-based decision-making. J Neurosci. 2011;31:16597–602.
Google Scholar
Robles CF, Johnson AW. Disruptions in effort-based decision-making and consummatory behavior following antagonism of the dopamine D2 receptor. Behav Brain Res. 2017;320:431–9.
Google Scholar
Cools R, D’Esposito M. Inverted-U–shaped dopamine actions on human working memory and cognitive control. Biol Psychiatry. 2011;69:e113–e25.
Google Scholar
Floresco SB, Tse MTL, Ghods-Sharifi S. Dopaminergic and glutamatergic regulation of effort- and delay-based decision making. Neuropsychopharmacology. 2008;33:1966–79.
Google Scholar
Randall PA, Pardo M, Nunes EJ, Cruz LL, Vemuri VK, Makriyannis A, et al. Dopaminergic modulation of effort-related choice behavior as assessed by a progressive ratio chow feeding choice task: pharmacological studies and the role of individual differences. PLOS ONE. 2012;7:e47934.
Google Scholar
Niv Y, Daw ND, Joel D, Dayan P. Tonic dopamine: opportunity costs and the control of response vigor. Psychopharmacology. 2007;191:507–20.
Google Scholar
Bell JA, Kivimäki M, Bullmore ET, Steptoe A, MRC ImmunoPsychiatry Consortium, Carvalho LA. Repeated exposure to systemic inflammation and risk of new depressive symptoms among older adults. Transl Psychiatry. 2017;7:e1208.
Google Scholar
Beurel E, Toups M, Nemeroff CB. The bidirectional relationship of depression and inflammation: double trouble. Neuron. 2020;107:234–56.
Google Scholar
Carvalho LA, Bergink V, Sumaski L, Wijkhuijs J, Hoogendijk WJ, Birkenhager TK, et al. Inflammatory activation is associated with a reduced glucocorticoid receptor alpha/beta expression ratio in monocytes of inpatients with melancholic major depressive disorder. Transl Psychiatry. 2014;4:e344.
Google Scholar
Kappelmann N, Lewis G, Dantzer R, Jones PB, Khandaker GM. Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol Psychiatry. 2018;23:335–43.
Google Scholar
Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70:31–41.
Google Scholar
Tyring S, Gottlieb A, Papp K, Gordon K, Leonardi C, Wang A, et al. Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial. Lancet Lond Engl. 2006;367:29–35.
Google Scholar
Nicoletti R, Adolfo Porro C, Brighetti G, Monti D, Pagnoni G, Guido M, et al. Long-term effects of vaccination on attentional performance. Vaccine. 2004;22:3877–81.
Google Scholar
Allison DJ, Ditor DS. The common inflammatory etiology of depression and cognitive impairment: a therapeutic target. J Neuroinflammation. 2014;11:151.
Google Scholar
Giollabhui NM, Swistun D, Murray S, Moriarity DP, Kautz MM, et al. Executive dysfunction in depression in adolescence: the role of inflammation and higher body mass. Psychol Med. 2020;50:683–91.
Google Scholar
Husain MI, Chaudhry IB, Husain MO, Hodsoll J, Ansari MA, Naqvi HA, et al. Minocycline and celecoxib as adjunctive treatments for bipolar depression: a multicentre, factorial design randomised controlled trial. Lancet Psychiatry. 2020;7:515–27.
Google Scholar
Bai S, Guo W, Feng Y, Deng H, Li G, Nie H, et al. Efficacy and safety of anti-inflammatory agents for the treatment of major depressive disorder: a systematic review and meta-analysis of randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020;91:21–32.
Google Scholar
Osimo EF, Baxter LJ, Lewis G, Jones PB, Khandaker GM. Prevalence of low-grade inflammation in depression: a systematic review and meta-analysis of CRP levels. Psychol Med. 2019;49:1958–70.
Google Scholar
Miller AH, Pariante CM. Trial failures of anti-inflammatory drugs in depression. Lancet Psychiatry. 2020;7:837.
Google Scholar
Bekhbat M, Li Z, Mehta ND, Treadway MT, Lucido MJ, Woolwine BJ, et al. Functional connectivity in reward circuitry and symptoms of anhedonia as therapeutic targets in depression with high inflammation: evidence from a dopamine challenge study. Mol Psychiatry. 2022;27:4113–21.
Google Scholar
Felger JC, Hernandez CR, Miller AH. Levodopa reverses cytokine-induced reductions in striatal dopamine release. Int J Neuropsychopharmacol. 2015;18:pyu084.
Google Scholar
Capuron L, Pagnoni G, Drake DF, Woolwine BJ, Spivey JR, Crowe RJ, et al. Dopaminergic mechanisms of reduced basal ganglia responses to hedonic reward during interferon alfa administration. Arch Gen Psychiatry. 2012;69:1044–53.
Google Scholar
Felger JC, Treadway MT. Inflammation effects on motivation and motor activity: role of dopamine. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2017;42:216–41.
Google Scholar
Eisenberger NI, Berkman ET, Inagaki TK, Rameson LT, Mashal NM, Irwin MR. Inflammation-induced anhedonia: endotoxin reduces ventral striatum responses to reward. Biol Psychiatry. 2010;68:748–54.
Google Scholar
Vichaya EG, Hunt SC, Dantzer R. Lipopolysaccharide reduces incentive motivation while boosting preference for high reward in mice. Neuropsychopharmacology. 2014;39:2884–90.
Google Scholar
Nunes EJ, Randall PA, Estrada A, Epling B, Hart EE, Lee CA, et al. Effort-related motivational effects of the pro-inflammatory cytokine interleukin 1-beta: studies with the concurrent fixed ratio 5/ chow feeding choice task. Psychopharmacology. 2014;231:727–36.
Google Scholar
Yohn SE, Arif Y, Haley A, Tripodi G, Baqi Y, Müller CE, et al. Effort-related motivational effects of the pro-inflammatory cytokine interleukin-6: pharmacological and neurochemical characterization. Psychopharmacology. 2016;233:3575–86.
Google Scholar
Lasselin J, Treadway MT, Lacourt TE, Soop A, Olsson MJ, Karshikoff B, et al. Lipopolysaccharide alters motivated behavior in a monetary reward task: a randomized trial. Neuropsychopharmacology. 2017;42:801–10.
Google Scholar
Draper A, Koch RM, van der Meer JW, AJ Apps M, Pickkers P, Husain M, et al. Effort but not reward sensitivity is altered by acute sickness induced by experimental endotoxemia in humans. Neuropsychopharmacology. 2018;43:1107–18.
Google Scholar
Voss MW, Vivar C, Kramer AF, van Praag H. Bridging animal and human models of exercise-induced brain plasticity. Trends Cogn Sci. 2013;17:525–44.
Google Scholar
Belvederi Murri M, Pariante C, Mondelli V, Masotti M, Atti AR, Mellacqua Z, et al. HPA axis and aging in depression: systematic review and meta-analysis. Psychoneuroendocrinology. 2014;41:46–62.
Google Scholar
Knapen J, Van de Vliet P, Van Coppenolle H, David A, Peuskens J, Pieters G, et al. Comparison of changes in physical self-concept, global self-esteem, depression and anxiety following two different psychomotor therapy programs in nonpsychotic psychiatric inpatients. Psychother Psychosom. 2005;74:353–61.
Google Scholar
Haller N, Lorenz S, Pfirrmann D, Koch C, Lieb K, Dettweiler U, et al. Individualized web-based exercise for the treatment of depression: randomized controlled trial. JMIR Ment Health. 2018;5:e10698.
Google Scholar
Pickett K, Yardley L, Kendrick T. Physical activity and depression: a multiple mediation analysis. Ment Health Phys Act. 2012;5:125–34.
Google Scholar
Wipfli B, Landers D, Nagoshi C, Ringenbach S. An examination of serotonin and psychological variables in the relationship between exercise and mental health. Scand J Med Sci Sports. 2011;21:474–81.
Google Scholar
White K, Kendrick T, Yardley L. Change in self-esteem, self-efficacy and the mood dimensions of depression as potential mediators of the physical activity and depression relationship: Exploring the temporal relation of change. Ment Health Phys Act. 2009;2:44–52.
Google Scholar
Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiatry. 2022;79:550–9.
Google Scholar
Dishman RK, McDowell CP, Herring MP. Customary physical activity and odds of depression: a systematic review and meta-analysis of 111 prospective cohort studies. Br J Sports Med. 2021;55:926–34.
Google Scholar
Singh B, Olds T, Curtis R, Dumuid D, Virgara R, Watson A, et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br J Sports Med. 2023;57:1203–9.
Google Scholar
Heissel A, Heinen D, Brokmeier LL, Skarabis N, Kangas M, Vancampfort D, et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br J Sports Med. 2023;57:1049–57.
Google Scholar
Recchia F, Bernal JDK, Fong DY, Wong SHS, Chung P-K, Chan DKC, et al. Physical activity interventions to alleviate depressive symptoms in children and adolescents: a systematic review and meta-analysis. JAMA Pediatr. 2023;177:132–40.
Google Scholar
Lee J, Gierc M, Vila-Rodriguez F, Puterman E, Faulkner G. Efficacy of exercise combined with standard treatment for depression compared to standard treatment alone: A systematic review and meta-analysis of randomized controlled trials. J Affect Disord. 2021;295:1494–511.
Google Scholar
Stothart CR, Simons DJ, Boot WR, Kramer AF. Is the effect of aerobic exercise on cognition a placebo effect? PLoS ONE. 2014;9:e109557.
Google Scholar
Plessen CY, Karyotaki E, Miguel C, Ciharova M, Cuijpers P. Exploring the efficacy of psychotherapies for depression: a multiverse meta-analysis. BMJ Ment Health. 2023;26. https://doi.org/10.1136/bmjment-2022-300626.
Edwards MK, Loprinzi PD. Effects of a sedentary behavior-inducing randomized controlled intervention on depression and mood profile in active young adults. Mayo Clin Proc. 2016;91:984–98.
Google Scholar
Endrighi R, Steptoe A, Hamer M. The effect of experimentally induced sedentariness on mood and psychobiological responses to mental stress. Br J Psychiatry J Ment Sci. 2016;208:245–51.
Google Scholar
Ross RE, VanDerwerker CJ, Saladin ME, Gregory CM. The role of exercise in the treatment of depression: biological underpinnings and clinical outcomes. Mol Psychiatry. 2023;28:298–328.
Google Scholar
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR et al. Exercise for depression. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD004366.pub6.
Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: a meta-analysis. J Affect Disord. 2016;202:67–86.
Google Scholar
Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res. 2016;77:42–51.
Google Scholar
Busch AM, Ciccolo JT, Puspitasari AJ, Nosrat S, Whitworth JW, Stults-Kolehmainen M. Preferences for exercise as a treatment for depression. Ment Health Phys Act. 2016;10:68–72.
Google Scholar
Carpiniello B, Primavera D, Pilu A, Vaccargiu N, Pinna F. Physical activity and mental disorders: a case–control study on attitudes, preferences and perceived barriers in Italy. J Ment Health. 2013;22:492–500.
Google Scholar
Fraser SJ, Chapman JJ, Brown WJ, Whiteford HA, Burton NW. Physical activity attitudes and preferences among inpatient adults with mental illness. Int J Ment Health Nurs. 2015;24:413–20.
Google Scholar
Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med. 2016;46:2869–81.
Google Scholar
Padin AC, Wilson SJ, Bailey BE, Malarkey WB, Lustberg MB, Farrar WB, et al. Physical activity after breast cancer surgery: does depression make exercise feel more effortful than it actually is? Int J Behav Med. 2019;26:237–46.
Google Scholar
Hsu F-C, Kritchevsky SB, Liu Y, Kanaya A, Newman AB, Perry SE, et al. Association between inflammatory components and physical function in the health, aging, and body composition study: a principal component analysis approach. J Gerontol A Biol Sci Med Sci. 2009;64:581–9.
Google Scholar
Severinsen MCK, Pedersen BK. Muscle-organ crosstalk: the emerging roles of myokines. Endocr Rev. 2020;41:bnaa016.
Google Scholar
Kistner TM, Pedersen BK, Lieberman DE. Interleukin 6 as an energy allocator in muscle tissue. Nat Metab. 2022;4:170–9.
Google Scholar
Chow LS, Gerszten RE, Taylor JM, Pedersen BK, van Praag H, Trappe S, et al. Exerkines in health, resilience and disease. Nat Rev Endocrinol. 2022;18:273–89.
Google Scholar
Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017;127:1–4.
Google Scholar
Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol. 2010;72:219–46.
Google Scholar
Samaras K, Botelho NK, Chisholm DJ, Lord RV. Subcutaneous and visceral adipose tissue gene expression of serum adipokines that predict type 2 diabetes. Obes Silver Spring Md. 2010;18:884–9.
Google Scholar
Verheggen RJHM, Maessen MFH, Green DJ, Hermus ARMM, Hopman MTE, Thijssen DHT. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue. Obes Rev. 2016;17:664–90.
Google Scholar
Beavers KM, Brinkley TE, Nicklas BJ. Effect of exercise training on chronic inflammation. Clin Chim Acta Int J Clin Chem. 2010;411:785–93.
Google Scholar
Chang E, Varghese M, Singer K. Gender and sex differences in adipose tissue. Curr Diab Rep. 2018;18:69.
Google Scholar
Evans J, Salamonsen LA. Inflammation, leukocytes and menstruation. Rev Endocr Metab Disord. 2012;13:277–88.
Google Scholar
Sacher J, Okon-Singer H, Villringer A. Evidence from neuroimaging for the role of the menstrual cycle in the interplay of emotion and cognition. Front Hum Neurosci. 2013;7:374.
Google Scholar
McNulty KL, Elliott-Sale KJ, Dolan E, Swinton PA, Ansdell P, Goodall S, et al. The effects of menstrual cycle phase on exercise performance in eumenorrheic women: a systematic review and meta-analysis. Sports Med. 2020;50:1813–27.
Google Scholar
Falconer CL, Cooper AR, Walhin JP, Thompson D, Page AS, Peters TJ, et al. Sedentary time and markers of inflammation in people with newly diagnosed type 2 diabetes. Nutr Metab Cardiovasc Dis. 2014;24:956–62.
Google Scholar
Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur Heart J. 2011;32:590–7.
Google Scholar
Nimmo MA, Leggate M, Viana JL, King JA. The effect of physical activity on mediators of inflammation. Diabetes Obes Metab. 2013;15:51–60.
Google Scholar
Paolucci EM, Loukov D, Bowdish DME, Heisz JJ. Exercise reduces depression and inflammation but intensity matters. Biol Psychol. 2018;133:79–84.
Google Scholar
Metsios GS, Moe RH, Kitas GD. Exercise and inflammation. Best Pract Res Clin Rheumatol. 2020;34:101504.
Google Scholar
Kohut ML, McCann DA, Russell DW, Konopka DN, Cunnick JE, Franke WD, et al. Aerobic exercise, but not flexibility/resistance exercise, reduces serum IL-18, CRP, and IL-6 independent of beta-blockers, BMI, and psychosocial factors in older adults. Brain Behav Immun. 2006;20:201–9.
Google Scholar
Marques A, Marconcin P, Werneck A, Ferrari G, Gouveia E, Kliegel M, et al. Bidirectional association between physical activity and dopamine across adulthood-a systematic review. Brain Sci. 2021. https://doi.org/10.3390/brainsci11070829.
Wu S-Y, Wang T-F, Yu L, Jen CJ, Chuang J-I, Wu F-S, et al. Running exercise protects the substantia nigra dopaminergic neurons against inflammation-induced degeneration via the activation of BDNF signaling pathway. Brain Behav Immun. 2011;25:135–46.
Google Scholar
Hattori S, Naoi M, Nishino H. Striatal dopamine turnover during treadmill running in the rat: relation to the speed of running. Brain Res Bull. 1994;35:41–49.
Google Scholar
Saanijoki T, Nummenmaa L, Tuulari JJ, Tuominen L, Arponen E, Kalliokoski KK, et al. Aerobic exercise modulates anticipatory reward processing via the μ-opioid receptor system. Hum Brain Mapp. 2018;39:3972–83.
Google Scholar
Bothe N, Zschucke E, Dimeo F, Heinz A, Wüstenberg T, Ströhle A. Acute exercise influences reward processing in highly trained and untrained men. Med Sci Sports Exerc. 2013;45:583–91.
Google Scholar
Crabtree DR, Chambers ES, Hardwick RM, Blannin AK. The effects of high-intensity exercise on neural responses to images of food. Am J Clin Nutr. 2014;99:258–67.
Google Scholar
Brush CJ, Hajcak G, Bocchine AJ, Ude AA, Muniz KM, Foti D, et al. A randomized trial of aerobic exercise for major depression: examining neural indicators of reward and cognitive control as predictors and treatment targets. Psychol Med. 2022;52:893–903.
Google Scholar
Wardle MC, Lopez-Gamundi P, LaVoy EC. Effects of an acute bout of physical exercise on reward functioning in healthy adults. Physiol Behav. 2018;194:552–9.
Google Scholar
Bernacer J, Martinez-Valbuena I, Martinez M, Pujol N, Luis EO, Ramirez-Castillo D, et al. An amygdala-cingulate network underpins changes in effort-based decision making after a fitness program. NeuroImage. 2019;203:116181.
Google Scholar
Leventhal AM. Relations between anhedonia and physical activity. Am J Health Behav. 2012;36:860–72.
Google Scholar
Soini E, Rosenström T, Määttänen I, Jokela M. Physical activity and specific symptoms of depression: a pooled analysis of six cohort studies. J Affect Disord. 2024;348:44–53.
Google Scholar
Sun C-W, Wang Y-J, Fang Y-Q, He Y-Q, Wang X, So BCL, et al. The effect of physical activity on anhedonia in individuals with depressive symptoms. PsyCh J. 2022;11:214–26.
Google Scholar
Lakes K. The response to challenge scale (RCS): the development and construct validity of an observer-rated measure of children’s self-regulation. Int J Educ Psychol Assess. 2012;10:83–96.
Google Scholar
Lakes KD, Hoyt WT. Promoting self-regulation through school-based martial arts training. J Appl Dev Psychol. 2004;25:283–302.
Google Scholar
Toups M, Carmody T, Greer T, Rethorst C, Grannemann B, Trivedi MH. Exercise is an effective treatment for positive valence symptoms in major depression. J Affect Disord. 2017;209:188–94.
Google Scholar
Chaddock-Heyman L, Erickson K, Voss M, Knecht A, Pontifex M, Castelli D, et al. The effects of physical activity on functional MRI activation associated with cognitive control in children: a randomized controlled intervention. Front Hum Neurosci. 2013;7. Accessed 8 Jan 2023.
Wu X, Lin P, Yang J, Song H, Yang R, Yang J. Dysfunction of the cingulo-opercular network in first-episode medication-naive patients with major depressive disorder. J Affect Disord. 2016;200:275–83.
Google Scholar
Crum J, Ronca F, Herbert G, Funk S, Carmona E, Hakim U, et al. Decreased exercise-induced changes in prefrontal cortex hemodynamics are associated with depressive symptoms. Front Neuroergonomics. 2022;3. Accessed 29 Mar 2023.
Colcombe SJ, Kramer AF, Erickson KI, Scalf P, McAuley E, Cohen NJ, et al. Cardiovascular fitness, cortical plasticity, and aging. Proc Natl Acad Sci USA. 2004;101:3316–21.
Google Scholar
Krafft CE, Schwarz NF, Chi L, Weinberger AL, Schaeffer DJ, Pierce JE, et al. An 8-month randomized controlled exercise trial alters brain activation during cognitive tasks in overweight children. Obesity. 2014;22:232–42.
Google Scholar
Etnier JL, Nowell PM, Landers DM, Sibley BA. A meta-regression to examine the relationship between aerobic fitness and cognitive performance. Brain Res Rev. 2006;52:119–30.
Google Scholar
Karrer TM, Josef AK, Mata R, Morris ED, Samanez-Larkin GR. Reduced dopamine receptors and transporters but not synthesis capacity in normal aging adults: a meta-analysis. Neurobiol Aging. 2017;57:36–46.
Google Scholar
Nordin K, Gorbach T, Pedersen R, Panes Lundmark V, Johansson J, Andersson M, et al. DyNAMiC: a prospective longitudinal study of dopamine and brain connectomes: A new window into cognitive aging. J Neurosci Res. 2022;100:1296–320.
Google Scholar
Karalija N, Johansson J, Papenberg G, Wåhlin A, Salami A, Köhncke Y, et al. Longitudinal dopamine D2 receptor changes and cerebrovascular health in aging. Neurology. 2022;99:e1278–e89.
Google Scholar
Contreras-Osorio F, Ramirez-Campillo R, Cerda-Vega E, Campos-Jara R, Martínez-Salazar C, Reigal RE, et al. Effects of physical exercise on executive function in adults with depression: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19:15270.
Google Scholar
Dotson VM, Gradone AM, Bogoian HR, Minto LR, Taiwo Z, Salling ZN. Be fit, be sharp, be well: the case for exercise as a treatment for cognitive impairment in late-life depression. J Int Neuropsychol Soc. 2021;27:776–89.
Google Scholar
Buschert V, Prochazka D, Bartl H, Diemer J, Malchow B, Zwanzger P, et al. Effects of physical activity on cognitive performance: a controlled clinical study in depressive patients. Eur Arch Psychiatry Clin Neurosci. 2019;269:555–63.
Google Scholar
Brüchle W, Schwarzer C, Berns C, Scho S, Schneefeld J, Koester D, et al. Physical activity reduces clinical symptoms and restores neuroplasticity in major depression. Front Psychiatry. 2021;12:660642.
Google Scholar
Drinkwater C, Wildman J, Moffatt S. Social prescribing. BMJ. 2019;364:l1285.
Google Scholar
Glowacki K, Duncan MJ, Gainforth H, Faulkner G. Barriers and facilitators to physical activity and exercise among adults with depression: a scoping review. Ment Health Phys Act. 2017;13:108–19.
Google Scholar